Has encephalitis been classified as polio/AFP, and vice versa?
The failure of JE vaccines in India in controlling AES incidence
Supplement – Polio Immunization, 1995-2020
Figures
Figure 2: AES Cases - 1993 to 2022
Figure 3: Japanese Encephalitis Cases: Old vs. New Methodology
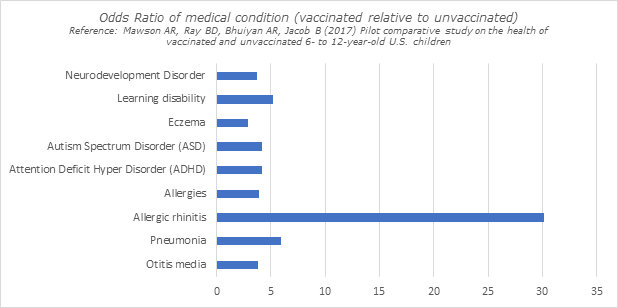
Figure 4: Health outcomes - Vaccinated vs. Unvaccinated Children
Summary
Encephalitis is a serious medical condition in which the brain becomes inflamed and the condition is characterized by an acute onset of fever and clinical neurological manifestation that includes mental confusion, disorientation, delirium, or coma. It is also associated with several negative long term health consequences such as developmental delay, ADHD, behavioural changes, learning disability, epilepsy, depression, anxiety, autism, schizophrenia and unprovoked seizures.
Based on surveillance numbers available since 1993, we have highlighted the below in this paper
There is a strong temporal association between rising incidence of AES (acute encephalitis syndrome) and increasing number of vaccinations. The first major outbreak since 1993 occurred in 2005, around the same time when India ran intensified pulse polio campaigns to “eliminate” polio by the then target of 2005.
Following the 2005 outbreak, Japanese encephalitis vaccinations were introduced in 11 endemic districts in 2006, and by 2011, the vaccine was introduced in 181 endemic districts. The reason for introducing this vaccine was based on the presumption that most if not all AES cases were due to Japanese encephalitis (JE), and hence introducing the JE vaccine in endemic regions will bring down the total burden of AES (it is noticeable that all AES cases before 2007 were reported as JE cases). At the same time, in 2006, WHO introduced a new methodology for JE diagnosis which, as was demonstrated in later years, only accounted for 14-15% of the total AES burden. However, AES incidence continued to rise even after introduction of JE vaccines, and in 2019, the AES incidence was more than twice as high as the outbreak in 2005, a clear indication of the failure of vaccines in bringing down incidence.
The increase in AES incidence is also temporally associated with the introduction of other vaccines in UIP such as pentavalent, measles (second dose), rubella, rotavirus etc. As more vaccines have been added we have seen increase in AES incidence. It is possible that simultaneous administration of several vaccines together further exacerbated the problem of rising AES. Conversely, when vaccination rates dropped in 2020 and 2021, a significant drop in AES incidence is also observed.
The temporal association of vaccines and AES is further accentuated by the fact that encephalitis is a known side effect of vaccines such as MMR & DPT which are mass administered. Additionally, there is literature highlighted in this writeup that shows that encephalitis cases were reported following administration of other vaccines such as polio and yellow fever.
This writeup also demonstrates that there is some overlap between diagnosis of encephalitis and polio, and that about 3%-16% cases of acute flaccid paralysis (which pre-1997 were classified as polio in India) are reported as encephalitis/AES in a couple of studies. Given that it was argued by this author in another writeup before, that the rise in AFP was likely triggered by mass polio vaccinations, and that we observe a similar temporal relationship with rise in AES, a further argument has been made that the initial AES outbreaks in the 2005-2012 timeframe (before newer vaccines were introduced to UIP) may have been triggered by mass polio vaccination campaigns. It raises the question that whether the unacknowledged negative effects of polio vaccination were, for the most part, wrongly attributed to the JE virus leading to the introduction of the JE vaccines.
The JE vaccines themselves have been associated with deaths based on media reports. Given the severely inadequate state of AEFI in India, no reasonable assessment can be made about the breadth & frequency of side effects, which is all the more reason to question indiscriminate mass vaccinations.
To sum up, a question needs to be raised about vaccinations in general. The rise in encephalitis is just one example of the long list of alleged vaccine harms. Additionally, given the association of encephalitis to several acute & chronic medical conditions, it also provides one possible explanation about why so many medical conditions are possibly associated with vaccines and hence classified as vaccine injuries.
1. The association between rise in Acute Flaccid Paralysis (AFP) and rise in Acute Encephalitis syndrome
Following the World Health Assembly declaration in 1988, to which India was a signatory, India committed to eradicating polio by 2000. Pulse polio campaigns were introduced in 1995. When the deadline was not met, it was further extended twice, to 2002 and 2005. In 2003, India executed it's largest ever polio campaign until then. This was further intensified in 2005 and with many children receiving 10 doses a year and few receiving upto 25 doses. This was performed with hardly any safety studies. As polio vaccination campaigns intensified, there was a record rise in cases of AFP (acute flaccid paralysis), which pre-1997 used to be classified as polio. However, something else noticeable happened in this period, and it's worthwhile to question it's link to the polio vaccinations. [1,2,3]
India's cases of AES (acute encephalitis syndrome) increased almost in sync with the increase in AFP cases. As of February 2012, India had recorded its highest number of AES cases in 2005 and 2011, in the same time period when India observed increasingly high cases of AFP following India's accelerated polio vaccination campaigns. With over 60,000 reported cases, 2011 & 2012 represent the highest number of annual AFP cases recorded in India. [4,5,6]. We will explore the link between polio, encephalitis and vaccines in general in the following sections.
Figure 1: AES vs. AFP
2. What is encephalitis?
Encephalitis is brain inflammation associated with acute and chronic medical conditions. Some snippets are as below:
“Encephalitis encompasses a broad range of pathophysiologic processes that result in inflammation of the brain parenchyma” [91]
“Acute encephalitis syndrome (AES) is characterized by an acute onset of fever and clinical neurological manifestation that includes mental confusion, disorientation, delirium, or coma” .... “The causative agent of AES varies with season and geographical location, and predominantly affects population below 15 years “ [24]
“Epidemic encephalitis (encephalitis lethargica, nona) may be defined as an epidemic syndrome characterized in most instances by a gradual onset with headache, vertigo, disturbances of vision, ocular palsies, changes in speech, dysphagia, marked asthenia, fever (usually of a low grade), obstinate constipation, incontinence of urine, a peculiar mask-like expression of the face, and a state of lethargy which gradually develops in the majority of the recognized cases into a coma that is more or less profound.” [33]
It is important to note that while encephalitis is characterised by acute onset of fever and neurological issues following brain inflammation, it’s etiology is unknown in majority of the cases [21]. Given that the etiological agent is not identified in majority of encephalitis cases, it is unclear as to how modern medicine has deduced viruses as the cause of encephalitis. Even if a virus is detected through tests, how is the causal link with the clinical manifestation of a disease established? The same question applies to viral transmission through vectors such as mosquitoes. Are there other factors such as suppression of immunity due to vaccines that are possibly exacerbating a relatively benign infection? It is hard to find studies that look at the prevalence of encephalitis in vaccinated versus unvaccinated population in endemic regions like India, however we do know from literature that vaccines can trigger encephalitis, and we have also observed in the rise in acute encephalitis syndrome following aggressive mass polio immunization campaigns.
“The magnitude of the problem of encephalitis is difficult to assess because of a lack of uniform definitions” [21]
"Many conditions mimic AES with difficulties in diagnosis of viral agents in India" [23]
"AES cases in India has not restricted itself to the JE aetiology. This is the biggest challenge clinicians in the field are facing" [24]
“A wide variety of infectious and non-infectious etiologies are associated with AES/encephalitis. However, in both Western industrialized nations and developing countries, the cause in more than half of cases remains unexplained despite extensive testing.” [21]
In California, in a study of 1570 suspected patients “Only 16% of patients had a confirmed or probable etiologic agent identified” [21]
“In a study on VE in Chinese children, the etiology was confirmed in 52.5% of patients.” [21]
3. Has encephalitis been classified as polio/AFP, and vice versa?
There is considerable literature to suggest that at least some of the encephalitis cases were traditionally diagnosed as polio clinically and that both these diseases were clinically difficult to differentiate.
In a writeup in Journal of Indian Pediatrics, the author emphasized that AFP due to JEV (Japanese Encephalitis Virus) is clinically similar to polio. "Japanese encephalitis virus, which is known to produce severe meningo-encephalomyelitis, should also be considered in the differential diagnosis of patients with polio-like illness in endemic areas." “In endemic areas like India where Japanese encephalitis as well as poliomyelitis still have a very high incidence, it will be difficult to differentiate between these two diseases on clinical grounds alone “ [9]
Japanese B encephalitis was listed as one of over 50 different diseases that were diagnosed as polio in an article in Illinois medical Journal in 1950 [8]
A writeup in Lancet in 1998 studying AFP in 22 Vietnamese children acknowledged that Japanese Encephalitis Virus causes AFP in children which has similar clinical and pathological features to poliomyelitis [10]
A 1929 writeup on Encephalitis emphasized the similarity between polio and encephalitis and observed that certain cases of poliomyelitis that are diagnosed as encephalitic type of poliomyelitis will likely be considered as cases of epidemic encephalitis. It identified poliomyelitis as a "like form of encephalitis lethargica (also called Japanese A encephalitis)" that occurred in younger patients. It also emphasized a case study of 12 patients who were diagnosed with poliomyelitis, as likely cases of epidemic encephalitis. [13]
It was observed in the first international poliomyelitis conference in 1949 that encephalitis caused confusion in a differential diagnosis of poliomyelitis. [14]
A study of AFP cases in a tertiary care hospital in Delhi from 2011 to 2013 reported that 3% of the AFP cases were encephalitis or meningoencephalitis. [7]
An analysis of 678 cases diagnosed as AFP in Malaysia from 2002 to 2007, published in The South East Asian Journal of Tropical Medicine and Public Health, observed that over 16% of AFP cases were viral encephalitis or meningitis/meningoencephalitis. An additional 16.5% suffered brain conditions, including encephalomyelitis and ADEM (acute demyelinating encephalomyelitis) among others. [90]
A 1938 writeup in the Journal of Experimental Medicine acknowledged that polio and different types of encephalitis such as Japanese encephalitis were clinically difficult to differentiate [15]
A writeup in “Annals of Indian Academy of Neurology” observed that "Japanese encephalitis is an encephalomyelitis and anterior horn cell involvement simulates polio myelitis-like illness" [26]
A 1962 writeup regarding Cincinnati’s Poliomyelitis Immunization and Surveillance Program in 1961 observed that 5 out of 56 polio like cases were encephalitis. [27]
Pre-1997 in India, all AFP cases were recorded as polio, with no standard case definition. [1] It is possible that many of the cases that would’ve been classified as polio pre-1997 were reclassified as acute encephalitis syndrome or AES after 2006 following change in definition of Japanese Encephalitis and introduction of the term AES.
4. Do vaccines cause AES?
Vaccines can cause encephalitis and encephalopathy, both of which are included in the broader definition of AES [16]. Below are a few examples:
OPV (Oral Polio Vaccine) and encephalitis
“Between 1964 and 1974 165,000 children born in Hamburg, were immunised thrice with OPV. In this period 19 convulsions and 3 permanent convulsive disorders were observed (1 case per 8,600 vaccinees; 1 convulsive disorder per 55,000 vaccinees)." [28]
“15 cases of encephalitis, several of these "acute infective encephalitis" were reported after polio vaccination”. [29]
Following 5 cases of encephalopathy/encephalitis in Bhutan in 2009, pentavalent vaccination was suspended. [32]
Both encephalitis and encephalopathy are listed as a post vaccine injuries due to MMR/DPT/DTap, eligible for vaccine compensation in US’ Vaccine Injury table [34]. Several vaccine victims and their families have been compensated for pos-vaccinal encephalitis/encephalopathy. [79]
A 1929 writeup on epidemic encephalitis discussed in detail several references of post vaccinal encephalitis following smallpox vaccination. [35]
9 deaths of children under 1 year of age due to encephalitis following smallpox vaccination were reported in the British Medical Journal in 1959. [88]
There are several references regarding encephalitis following yellow fever vaccination.
Three instances of infants developing encephalitis following yellow fever vaccination were reported in 1954. [86]
4 cases of children developing encephalitis following yellow fever vaccination were reported in 1955. [85]
Another case was reported in 1954. [87]
In 1952, it was reported that a baby developed meningo-encephalitis following yellow fever vaccination. [88]
Given the sustained increase in AES following polio immunizations, and the continued rise following introduction of several new vaccines in the immunization schedule such as pentavalent, rotavirus, rubella, 2nd dose of measles etc., it is plausible to suggest that vaccines have played a role in this epidemic of AES in India. [3, 42, 43, 44, 45, 46, 47, 48. 49, 50, 51, 52, 53, 54]
Figure 2: AES Cases - 1993 to 2022
5. The failure of JE vaccines in India in controlling AES incidence
Up until 2005, all cases of AES were reported as JE (Japanese Encephalitis) cases. In 2006, the World Health Organization coined the term “acute encephalitis syndrome” (AES) for the purpose of surveillance of JE. [21] Both PATH (2005) and WHO (2007) had reported total AES numbers as JE numbers, despite the fact that based on the new definition since 2006, JE constituted only about 14%-15% of the total burden of AES. [40, 80]. Published studies also reported AES numbers as JE numbers [81, 82] back then.
In 2005, it was reported that India had recorded a massive JE outbreak, justifying the introduction of JE vaccines in endemic regions. Since the 2005 outbreak was used as justification for introducing JE vaccines, the expectation would be that after the introduction of JE vaccines, the overall incidence of JE (based on the pre-2006 definition) would decrease. However, as shown in the chart below, this clearly was not the case, and in fact, in 2019, the total incidence of JE (pre-2006 definition, AES since 2006) was almost 2 & a half times as high as the incidence in 2005. It is odd that the definition of JE was changed in 2006 by WHO, in the same year when the JE vaccine was launched in India. This approach of change in definition to give the illusion of decline in disease incidence sounds very similar to the approach used to redefine polio in 1997, with many of the diseases that would’ve been classified as polio pre-1997 now classified as AFP (acute flaccid paralysis).
“The diagnosis and management of encephalitis were previously largely based on clinical grounds and minimal laboratory investigations. Japanese encephalitis (JE) gets considered as the probable diagnosis in most encephalitis cases” [35]
Figure 3: Japanese Encephalitis Cases: Old vs. New Methodology
*Data Sources AES/JE incidence: [4, 36, 37, 38, 39, 40]
The JE vaccines have not helped in changing the epidemiology of JE or AES in India, and India is actually recording more cases of AES. Vaccine efficacy studies have demonstrated limited efficacy of 35%, and even these studies either ignore or only passively acknowledge that JE vaccines have not helped in reducing the burden of AES. Moreover, none of the studies explore the possible link between mass vaccination campaigns and rise in AES. [5, 16, 17, 22, 25]
“A slight increase in the incidence of both JE and AES in Maharashtra was seen in the post-JE vaccine two-dose-schedule implementation period during 2014–2020 in comparison to
the earlier period using a single dose implemented during 2007–2013” [17]
Over time, despite no noticeable drop in AES, it has been observed that majority of AES are not JE [18]
"Since 2005, the overall incidence of acute encephalitis syndrome in India has not decreased, with 10,867–13,672 cases reported each year to the NVBDCP between 2014 and 20173 Among reported cases of acute encephalitis syndrome, only 14–18% are associated with JEV infection and the aetiology of most cases in India remain unknown" [19]
"Since 2009, the incidence of AES and JE cases has been increasing in Bihar." (despite introduction of the JE vaccine) [20]
6. Side effects of JE vaccines
In Taiwan, a case was reported of an adult suffering from AFP following JEV infection despite having received 4 does of the JE vaccine in childhood [11]
Severe side effects following JE vaccination were reported in both Japan and Denmark. Denmark especially reported a very high incidence of acute disseminated encephalomyelitis following Japanese encephalitis vaccination (1 in 50,000-75,000 vaccinees).
"Approximately 10% of those administered Japanese encephalitis vaccine reported systemic reactions, such as fever, headache, malaise and rash. Serious adverse events include hypersensitivity-type reactions and neurological reactions. A review of postmarketing data in Japan from 1996 to 1998 revealed 17 neurological disorders after the administration of approximately 9.4 million doses of Japanese encephalitis vaccine. Among those, 16 cases had meningitis or meningoencephalitis, including ®ve probable cases of acute disseminated encephalomyelitis (0.2 per 100 000 vaccinations). In Denmark, acute disseminated encephalomyelitis following Japanese encephalitis vaccination occurred more frequently, at approximately 1 in 50 000± 5 000 vaccinees " [12]
“According to the vaccine manufacturer, the following side effects have been reported following receipt of the Japanese encephalitis vaccine: flu-like symptoms, including fever, headache, malaise, rash, chills, dizziness, myalgia, nausea, vomiting and abdominal pain. Other reported reactions include: hives and facial swelling, joint swelling, generalized itching, respiratory distress, Guillain-Barré syndrome, renal failure, seizures, encephalitis, encephalopathy, transverse myelitis, optic neuritis, cranial nerve paresis, cerebellar ataxia, Bell's palsy, fatal myocarditis and sudden death. Some of these reactions occurred following receipt of the Japanese encephalitis vaccine concurrent with other vaccines.” [30]
“It is worth investigating the association between JE vaccination and anti-NMDA receptor encephalitis “ [31]
3 deaths following JE vaccinations in school aged children was reported in 2015 in Tripura.
3 babies died following measles and Japanese Encephalitis vaccination in Bihar in 2017. The families were given compensation in 2024.
4 babies died following measles and Japanese Encephalitis vaccination in Jharkhand in 2018.
In neighbouring Myanmar, 3 school aged children died following JE vaccination.
In 2006, in UP, it was reported that most of the children who had died due to encephalitis had been vaccinated for JE.
Besides the above, there are several negative long term health consequences of encephalitis covered in the next section.
7. Long term health outcomes following encephalitis
Encephalitis is associated with several negative long term health consequences such as developmental delay, ADHD, behavioural changes, learning disability, epilepsy, depression, anxiety and autism. Encephalitis is also sometimes accompanied with seizures, and seizures have been associated with mental health issues in the long term such as schizophrenia. [91]
“Autism can be characterized as chronic low grade encephalopathy” [63]
According to a meta analysis of 16 studies, encephalitis during childhood is associated with long term side effects, including developmental delay, abnormal behaviour, motor impairment, and seizures.
“Incomplete recovery was reported in 312 children (42.0%; 95% confidence interval [CI] 31.6-53.1% in pooled estimate). Among the other sequelae, developmental delay, abnormal behaviour, motor impairment, and seizures were reported among 35.0% (95% CI 10.0-65.0%), 18.0% (95% CI 8.0-31.0%), 17.0% (95% CI 10.0-26.0%), and 10.0% (95% CI 6.0-14.0%) respectively” [64]
“Of 101 children enrolled (with history of encephalitis), 4 died and 25 had other neurological sequelae, including epilepsy, headache, developmental delay, and emotional or behavioral changes during the 5 years of follow-up” [65]
“most patients (with history of encephalitis) had persistent impairments, with frequent deficits in cognitive function, especially memory and attention. Depression and anxiety were also common” [66]
"many studies indicate that children with an ASD (autism) diagnosis have brain pathology suggestive of ongoing neuroinflammation or encephalitis" [67]
"Regression in AE (autoimmune encephalitis) Mimics Autistic Regression" [68]
“A clinical picture which is indistinguishable from infantile autism may develop after a brain disease such as encephalitis when it occurs in early childhood." [69]
“Encephalitis in children may be associated with significant long-term neurologic sequelae. Significant cognitive impairment, attention-deficit/hyperactivity disorder, and learning disabilities are common, and even children who were considered fully recovered at discharge may be significantly affected” [70]
“Persisting symptoms after childhood encephalitis were present for a substantial number of children. Seizures increased the risk of subsequent epilepsy; the only other prognostic marker was admission to the ICU. Even children who were considered fully recovered at discharge reported persisting symptoms at follow-up evaluations” [71]
“31 (18%) were mildly impaired, 25 (14%) were severely impaired, and 3 (1%) were in a vegetative state. The most frequent symptoms were difficulty concentrating (42%), behavioral disorders (27%), speech disorders (20%), and memory loss (19%). Fifteen of 63 patients (24%) previously employed were still unable to resume work” [72]
“Paediatric encephalitis is estimated to cause up to a 13% risk of death and 78% risk of neurological sequelae during 1 to 5 years of follow‐up” [73]
“We concluded that PEE (post encephalitic epilepsy) is not a rare complication of acute encephalitis” [74]
“ Encephalitis leads to significant morbidity and death, and incomplete recovery is achieved in the majority of hospitalized patients.” [75]
"Encephalitis can cause mental deficiency and loss of ability to walk & talk". [76]
“Patients with encephalitis risk developing seizures acutely, but also are more likely to develop later unprovoked seizures .... patients with encephalitis overall are about 16 times more likely than the general population to develop later unprovoked seizures”. [91]
Newborn encephalopathy (which can also be triggered by vaccines) is associated with autism. [77]
“Vaccine administration is the second leading cause of febrile seizures” [61]
“Children with epilepsy as well as febrile seizures - with and without concomitant epilepsy - are at elevated risk of developing a broad range of psychiatric disorders in later life.... The strongest associations were observed for schizophrenia and related disorders” [62]
Some of the negative long term health impacts due to encephalitis including developmental delay, learning disability, ASD and ADHD are also observed more frequently in vaccinated children compared to unvaccinated children, further underscoring the link between vaccinations and encephalitis [78]
Figure 4: Health outcomes - Vaccinated vs. Unvaccinated Children
8. Conclusion
The aggressive vaccination campaigns and never ending addition of new vaccines to UIP since the turn of the century, occurring in tandem with rising incidence of AES (acute encephalitis syndrome) is likely not a coincidence. AES incidence aside, newly introduced vaccines in India have been controversial for other reasons. For example, Dr. Pulliyel, former member of NTAGI (National Technical Advisory Group on Immunization) has argued that rotavirus vaccines actually increased incidence of diarrhea among vaccinated, and the pentavalent vaccine had resulted in higher all cause mortality compared to its predecessor - DPT [83, 84]. It can be argued that two of the largest vaccination drives in India’s history – polio & covid, have been controversial and counter-productive. JE is just another example of vaccination failure in curtailing incidence of AES. Are we in an era of man made epidemics negatively impacting society, especially children, and if so, and what are the steps needed to reverse this trend?
Supplement – Polio Immunization, 1995-2020
Polio campaigns intensified and peaked in the 2005-2011 timeframe. Below is a timeframe
1995-96 : First National Immunization Day (NID).
1996-97 : Second NID.
1997-98 : Third NID.
1998-99 : Fourth NID.
1999-00 : Intensified strategy introduced with Four Sub NIDs and Two NIDs. ‘House-to-House’ Immunization introduced.
2000-01 : Two Sub NIDs and two NIDs followed by ‘House-to-House’ Immunization.
2001-02 : Two NIDs and one Sub NID followed by ‘House-to-House’ Immunization .
2002-03 : Two NIDs and two Sub NIDs followed by ‘House-to-House’ Immunization.
2003-04 : Two NIDs and four Sub NIDs followed by House-to-House Immunisation.
2004 : Five NIDs, one Sub NID.
2005 : Two NIDs and six Sub NIDs.
2006 : Two NIDs and six Sub NIDs.
2007 : Two NIDs and Six Sub NIDs followed by House-to-House Immunization undertaken. One round every month in UP.
2008 : Three NIDs and Six Sub NIDs, followed by House-to-House and mop-ups.
2009 : One NID and Nine Sub NIDs, followed by House-to-House and mop-ups.
2010 : Two NIDs and Ten Sub NIDs, followed by House-to-House and mop-ups.
2011 : Two NIDs and Six Sub NIDs
2012 : Two NIDs and Four Sub NIDs
2013 : Two NIDs and Four Sub NIDs, followed by House-to-House and mop-ups wherever required.
2014 : Two NIDs and three Sub NIDs.
2018: 2 NIDs, 2 SNIDs.
2019, 2020: 1 NID and 2 SNIDs.
References
[1] Srivastava, Vratesh. “The Other Side of India’s Polio Eradication Story.” Vratesh’s Newsletter, 18 Nov. 2023, vratesh.substack.com/p/the-other-side-of-indias-polio-eradication. Accessed 9 Mar. 2024.
[2] Paul Y, Priya. Polio eradication in India: some observations. Vaccine. 2004 Oct 22;22(31-32):4144-8. doi: 10.1016/j.vaccine.2004.04.032. PMID: 15532129.
[3] World Health Organization. “India Launches Largest Ever Campaign to Tackle Polio Epidemic.” www.who.int, 5 Feb. 2003, www.who.int/news/item/05-02-2003-india-launches-largest-ever-campaign-to-tackle-polio-epidemic.
[4] Dwaipayan Adhya, Kallol Dutta, Anirban Basu, Japanese encephalitis in India: risk of an epidemic in the National Capital Region, International Health, Volume 5, Issue 3, September 2013, Pages 166–168, https://doi.org/10.1093/inthealth/iht015, https://academic.oup.com/inthealth/article/5/3/166/651920?login=false
[5] Srivastava, Neha, et al. “The Outbreaks of Acute Encephalitis Syndrome in Uttar Pradesh, India (1978–2020) and Its Effective Management: A Remarkable Public Health Success Story.” Frontiers in Public Health, vol. 9, 9 Feb. 2022, https://doi.org/10.3389/fpubh.2021.793268, https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2021.793268/full#T1
[6] World Health Organization. “AFP/Polio Data.” Who.int, WHO, 2023, extranet.who.int/polis/public/CaseCount.aspx. Accessed 2023.
[7] Kumar, Ajay. “A STUDY of ACUTE FLACCID PARALYSIS CASES REPORTED from a TERTIARY CARE HOSPITAL in DELHI.” Indian Journal of Child Health, vol. 02, no. 04, 25 Dec. 2015, pp. 165–168, https://doi.org/10.32677/ijch.2015.v02.i04.006, https://web.archive.org/web/20200615002155/https://mansapublishers.com/IJCH/article/view/550
[8] Illinois State Medical Society, and Library The New York Academy of Medicine. Illinois Medical Journal. Internet Archive, [Chicago: Illinois State Medical Society, 1889-1962], 1950, https://archive.org/details/illinoismedicalj98unse/page/n385/mode/2up
[9] Garg, Ravindra Kumar. “Indian Pediatrics - Editorial.”
http://Www.indianpediatrics.net
, Journal of Indian Pediatrics, Nov. 1998, http://www.indianpediatrics.net/nov1998/nov-1146-1148.htm.
[10] Solomon T, Kneen R, Dung NM, Khanh VC, Thuy TT, Ha DQ, Day NP, Nisalak A, Vaughn DW, White NJ. Poliomyelitis-like illness due to Japanese encephalitis virus. Lancet. 1998 Apr 11;351(9109):1094-7. doi: 10.1016/S0140-6736(97)07509-0. PMID: 9660579.
[11] Chung, CC., Lee,
http://S.SJ
., Chen, YS. et al. Acute Flaccid Paralysis as an Unusual Presenting Symptom of Japanese Encephalitis: A Case Report and Review of the Literature. Infection 35, 30–32 (2007). https://doi.org/10.1007/s15010-007-6038-7, https://link.springer.com/article/10.1007/s15010-007-6038-7
[12] Piyasirisilp, S., & Hemachudha, T. (2002). Neurological adverse events associated with vaccination. Current Opinion in Neurology, 15(3), 333–338. doi:10.1097/00019052-200206000-00018, https://sci-hub.se/10.1097/00019052-200206000-00018
[13] Matheson commission, and Internet Archive. Epidemic Encephalitis: Etiology, Epidemiology, Treatment; Internet Archive, Columbia University Press, 1 Jan. 1929, archive.org/details/epidemicencephal0000math/page/4/mode/2up?q=Poliomyelitis. Accessed 9 Mar. 2024.
[14] International poliomyelitis congress, and Internet Archive. Poliomyelitis Papers and Discussions Presented at the First International Poliomyelitis Conference. Internet Archive, International Poliomyelitis Congress, 1949, https://archive.org/details/poliomyelitispap0000inte/page/186/mode/2up
[15] Leslie Webster. “Japanese B Encephalitis Virus, It’s Differentiation from St. Louis Encephalitis Virus and Relationship to Louping Ill Virus.” Internet Archive, 1938, archive.org/details/in.ernet.dli.2015.232954/page/n195/mode/1up.
[16] Vashishtha, Vipin M., and V. G. Ramachandran. “Vaccination Policy for Japanese Encephalitis in India: Tread with Caution!” Indian Pediatrics, vol. 52, no. 10, Oct. 2015, pp. 837–839, https://doi.org/10.1007/s13312-015-0728-5, https://www.indianpediatrics.net/oct2015/837.pdf
[17] Tandale BV, Deshmukh PS, Tomar SJ, Narang R, Qazi MS, Goteti Venkata P, Jain M, Jain D, Guduru VK, Jain J, Gosavi RV, Valupadas CS, Deshmukh PR, Raut AV, Narlawar UW, Jha PK, Bondre VP, Sapkal GN, Damle RG, Khude PM, Niswade AK, Talapalliwar M, Rathod P, Balla PS, Muttineni PK, Kalepally Janakiram KK, Rajderkar SS. Incidence of Japanese Encephalitis and Acute Encephalitis Syndrome Hospitalizations in the Medium-Endemic Region in Central India. J Epidemiol Glob Health. 2023 Jun;13(2):173-179. doi: 10.1007/s44197-023-00110-7. Epub 2023 May 10. PMID: 37162636; PMCID: PMC10271976, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10271976/
[18] Ranjan P, Gore M, Selvaraju S, Kushwaha KP, Srivastava DK, Murhekar M. Changes in acute encephalitis syndrome incidence after introduction of Japanese encephalitis vaccine in a region of India. J Infect. 2014 Aug;69(2):200-2. doi: 10.1016/j.jinf.2014.03.013. Epub 2014 Mar 20. PMID: 24657663, https://www.researchgate.net/publication/234030375_Changing_landscape_of_acute_encephalitis_syndrome_in_India_A_systematic_review
[19] Ravi V, Hameed SKS, Desai A, Mani RS, Reddy V, Velayudhan A, Yadav R, Jain A, Saikia L, Borthakur AK, Sharma A, Mohan DG, Bhandopadhyay B, Bhattacharya N, Inamdar L, Hossain S, Daves S, Sejvar J, Dhariwal AC, Sen PK, Venkatesh S, Prasad J, Laserson K, Srikantiah P. An algorithmic approach to identifying the aetiology of acute encephalitis syndrome in India: results of a 4-year enhanced surveillance study. Lancet Glob Health. 2022 May;10(5):e685-e693. doi: 10.1016/S2214-109X(22)00079-1. PMID: 35427525, https://www.thelancet.com/action/showPdf?pii=S2214-109X%2822%2900079-1, https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(22)00079-1/fulltext
[20] Pisudde, PM, et al. “Status and Trend of Acute Encephalitis Syndrome and Japanese Encephalitis in Bihar, India.” The National Medical Journal of India, vol. 30, no. 6, 2017, p. 317, https://doi.org/10.4103/0970-258x.239070, https://nmji.in/status-and-trend-of-acute-encephalitis-syndrome-and-japanese-encephalitis-in-bihar-india/
[21] Kumar R. Understanding and managing acute encephalitis. F1000Res. 2020 Jan 29;9:F1000 Faculty Rev-60. doi: 10.12688/f1000research.20634.1. PMID: 32047620; PMCID: PMC6993835, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6993835/
[22] Deval, H, et al. “A Decade of Acute Encephalitis Syndrome (AES) Cases in Eastern Uttar Pradesh, India: Etiological Scenario and Preventive Strategies (2010–2019).” International Journal of Infectious Diseases, vol. 101, no. 101, 1 Dec. 2020, pp. 241–241, https://doi.org/10.1016/j.ijid.2020.11.066, https://www.ijidonline.com/article/S1201-9712(20)32385-7/fulltext
[23] Tandale, Babasaheb V., et al. “Infectious Causes of Acute Encephalitis Syndrome Hospitalizations in Central India, 2018–20.” Journal of Clinical Virology, vol. 153, 1 Aug. 2022, p. 105194, http://www.sciencedirect.com/science/article/pii/S1386653222001275, https://doi.org/10.1016/j.jcv.2022.105194
[24] Ghosh, Sourish, and Anirban Basu. “Acute Encephalitis Syndrome in India: The Changing Scenario.” Annals of Neurosciences, vol. 23, no. 3, 2016, pp. 131–133, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5043220/, https://doi.org/10.1159/000449177, https://karger.com/aon/article/23/3/131/43000/Acute-Encephalitis-Syndrome-in-India-The-Changing
[25] Kharya, Pradip, et al. “Japanese Encephalitis in Uttar Pradesh, India: A Situational Analysis.” Journal of Family Medicine and Primary Care, vol. 9, no. 7, 2020, p. 3716, https://doi.org/10.4103/jfmpc.jfmpc_449_20, https://journals.lww.com/jfmpc/Fulltext/2020/09070/Japanese_encephalitis_in_Uttar_Pradesh,_India__A.93.aspx
[26] Misra UK, Kalita J. Changing Spectrum of Acute Encephalitis Syndrome in India and a Syndromic Approach. Ann Indian Acad Neurol. 2022 May-Jun;25(3):354-366. doi: 10.4103/aian.aian_1117_21. Epub 2022 Jun 8. PMID: 35936627; PMCID: PMC9350753, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9350753/
[27] Cockburn, T. A., E. Russell Porter, Kenneth I. E. Macleod, Jan D. Litsey, & Charles C. Croft. (1962). Cincinnati’s Poliomyelitis Immunization and Surveillance Program in 1961. Public Health Reports (1896-1970), 77(7), 589–592. https://doi.org/10.2307/4591563, https://www.jstor.org/stable/4591563?read-now=1&seq=3#page_scan_tab_contents
[28] Ehrengut W, Ehrengut J. Convulsions following oral polio immunisation. Dev Biol Stand. 1979;43:165-71. PMID: 520668, https://pubmed.ncbi.nlm.nih.gov/520668/
[29] Miller, David L, and N S Galbraith. Surveillance of the Safety of Oral Poliomyelitis Vaccine in England and Wales 1962--4. Vol. 2, no. 5460, 28 Aug. 1965, pp. 504–509, https://doi.org/10.1136/bmj.2.5460.504, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1845665/pdf/brmedj02591-0015.pdf
[30] Miller, Neil Z., and Internet Archive. Vaccine Safety Manual for Concerned Families and Health Practitioners. Internet Archive, Santa Fe, N.M. : New Atlantean Press, 2008, archive.org/details/isbn_9781881217350/page/455/mode/1up.
[31] Wang H. Anti-NMDA Receptor Encephalitis and Vaccination. Int J Mol Sci. 2017 Jan 18;18(1):193. doi: 10.3390/ijms18010193. PMID: 28106787; PMCID: PMC5297824, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5297824/
[32] Passi, Gouri Rao. “PRIMUM NON NOCERE.” Journal of Indian Pediatrics, vol. 50, 15 Dec. 2013, https://indianpediatrics.net/dec2013/1165.pdf.
[33] H.F. Smith. Epidemic Encephalitis, Public Health Reports 1921-02-11: Vol 36 Iss 6. Internet Archive, SAGE PUBLICATIONS, INC., 11 Feb. 1921, archive.org/details/sim_public-health-reports_1921-02-11_36_6/mode/2up.
[34] Health Resources and Service Administration. “Vaccine Injury Table.” Www.hrsa.gov, www.hrsa.gov/vaccine-compensation/covered-vaccines.
[35] Tandale BV, Narang R, Vijay Kumar G, Jain M, Tomar SJ, Deshmukh PS. Infectious Causes of Acute Encephalitis Syndrome in India - Decadal Change and the Way Forward. Indian Pediatr. 2023 Sep 15;60(9):709-713. Epub 2023 May 30. PMID: 37260063. https://indianpediatrics.net/sep2023/709.pdf
[36] Tiwari, Sarika, et al. “Japanese Encephalitis: A Review of the Indian Perspective.” The Brazilian Journal of Infectious Diseases, vol. 16, no. 6, 1 Nov. 2012, pp. 564–573, www.sciencedirect.com/science/article/pii/S1413867012002073, https://doi.org/10.1016/j.bjid.2012.10.004.
[37] Singh Z, Agarwal VK. Japanese Encephalitis : Is Routine Immunization Required? Med J Armed Forces India. 2005 Oct;61(4):357-9. doi: 10.1016/S0377-1237(05)80066-8. Epub 2011 Jul 21. PMID: 27407808; PMCID: PMC4922931.
[38] Vashishtha VM. Encephalitis outbreaks in India: A cluttered landscape. Pediatric Infectious Disease. 2015 October-December;7(4):89–91. doi: 10.1016/j.pid.2015.11.008. Epub 2015 Dec 2. PMCID: PMC7148934.
[39] Singh, Amresh K., et al. “Recent Trends and Changing Aetiology of Acute Encephalitis Syndrome in India.” Asian Journal of Research in Infectious Diseases, 31 Jan. 2020, pp. 33–47, https://doi.org/10.9734/ajrid/2020/v3i130119.
[40] World Health Organization. “GHO | by Category | Japanese Encephalitis - Reported Cases by Country.” WHO, apps.who.int/gho/data/node.main.WHS3_42?lang=en.
[41] Ministry of Health & Family Welfare-Government of India. NATIONAL VECTOR BORNE DISEASE CONTROL PROGRAMME. 25 June 2011. https://cdn.who.int/media/docs/default-source/wrindia/kala-azar/12th-five-year-plan_national-vector-borne-disease-control-programme-india.pdf?sfvrsn=1bde00dc_2.
[42] Ministry of Health and Family Welfare. “Index4 :: Central Bureau of Health Intelligence.” Cbhidghs.mohfw.gov.in, 2005, cbhidghs.mohfw.gov.in/index4.php.
[43] Ministry of Health and Family Welfare. National Immunization Schedule (NIS) for Infants, Children and Pregnant Women. Ministry of Health and Family Welfare, 2023. https://main.mohfw.gov.in/sites/default/files/245453521061489663873.pdf.
[44] Government of India. “THREE NEW VACCINES INCLUDING INDIGENOUSLY DEVELOPED ROTAVIRUS VACCINE to BE PROVIDED to ALL INDIAN CHILDREN.” Pib.gov.in, 3 July 2014, pib.gov.in/newsite/PrintRelease.aspx?relid=106055.
[45] GAVI. “Pentavalent Vaccine Introductions Represent Historic Milestone for Immunisation in India.” Www.gavi.org, 1 Nov. 2014, www.gavi.org/news/media-room/pentavalent-vaccine-introductions-represent-historic-milestone-immunisation-india.
[46] Ministry of Health and Family Welfare, “Shri J P Nadda Launches Pneumococcal Conjugate Vaccine (PCV) under Universal Immunization Programme (UIP).” Web.archive.org, 18 May 2017, web.archive.org/web/20170518222209/pib.nic.in/newsite/PrintRelease.aspx?relid=161763.
[47] Paul, Sourabh; Sahoo, Jyotiranjan. Four New Vaccines for Routine Immunization in India: What About Hemophilus Influenza B and Pneumococcal Vaccine?. Journal of Family Medicine and Primary Care 4(1):p 9-12, Jan–Mar 2015. | DOI: 10.4103/2249-4863.152238, https://journals.lww.com/jfmpc/fulltext/2015/04010/four_new_vaccines_for_routine_immunization_in.3.aspx.
[48] Ministry of Health and Family Welfare. “Eradication of Polio.” Pib.gov.in, 10 Aug. 2018, pib.gov.in/Pressreleaseshare.aspx?PRID=1542730
[49] USAID, et al. POLIO Annual Report Fy18 CORE Group Polio Project. 2017, https://coregroup.org/wp-content/uploads/2019/02/CGPP-Annual-Report-FY18.pdf.
[50] World Health Organization, et al. Polio Eradication Initiative Global 2005 Annual Report. May 2006, https://polioeradication.org/wp-content/uploads/2016/07/AnnualReport2005_ENG.pdf.
[51] Paul, Yash. “Why Polio Has Not Been Eradicated in India despite Many Remedial Interventions?” Vaccine, vol. 27, no. 28, June 2009, pp. 3700–3703, https://doi.org/10.1016/j.vaccine.2009.03.078.
[52] Rotary International. “INDIA - POLIO ERADICATION FIGURES - Rotary International Operation Manual inside 2014-15 Final.” SlideShare, 16 June 2014, www.slideshare.net/PabloAmo/operation-mannual-inside-201415-final.
[53] World Health Organization. “WHO Immunization Data Portal.” Immunizationdata.who.int, immunizationdata.who.int.
[54] Ministry of Health and Family Welfare. “Japanese Encephalities :: National Center for Vector Borne Diseases Control (NCVBDC).” Web.archive.org, 15 Feb. 2023, web.archive.org/web/20230215074846/ncvbdc.mohfw.gov.in/index1.php?lang=1&level=1&sublinkid=5773&lid=3693. Accessed 24 Mar. 2024.
[55] Infoway, Tripura. “TRIPURAINFOWAY : Tripura’s Latest News, Views & IT Portal.” Www.tripurainfoway.com, 6 June 2015, www.tripurainfoway.com/news-details/TN/28976/3-children-die-after-je-vaccination-in-tripura-many-admitted-to-hospital-tripura-demands-central-expert-team-to-study-deaths.html.
[56] Mohit, Alok. “Two Children Die in Bihar after Being Administered Vaccine against Japanese Encephalitis, Measles.” Hindustan Times, 6 May 2017, www.hindustantimes.com/india-news/two-children-die-in-bihar-after-being-administered-vaccine-against-japanese-encephalitis-measles/story-a3pFN3Q6XQP1QSYGSuSHeN.html.
[57] Sharma, Vishal. “Four Infants Die after Taking Japanese Encephalitis Vaccine in Palamu.” Hindustan Times, 8 Apr. 2018, www.hindustantimes.com/ranchi/three-infants-die-hours-after-taking-japanese-encephalitis-vaccine-in-palamu/story-OTU5MPLN11BdiaMhWOkV9M.html.
[58] Zin, Salai Thant. “Girl, 10, Dies after Being Administered Encephalitis Vaccine.” The Irrawaddy, 23 Nov. 2017, www.irrawaddy.com/news/burma/girl-10-dies-administered-encephalitis-vaccine.html.
[59] Pritha, Chatterjee. “Children Deaths in Gorakhpur: A Dissolving Faith,an Enduring Mystery | the Indian Express.” Indian Express, 14 Aug. 2017, web.archive.org/web/20170814051711/indianexpress.com/article/news-archive/regional/children-deaths-in-gorakhpur-a-dissolving-faith-an-enduring-mystery.
[60] Hindustan Team. “टीकाकरण में मृत बच्चों के परिजनों को मिला मुआवजा.” Https://Www.livehindustan.com/, Live Hindustan, 19 Mar. 2024, www.livehindustan.com/bihar/muzaffarpur/story-families-of-children-who-died-during-vaccination-received-compensation-9574664.amp.html.
[61] Principi N, Esposito S. Vaccines and febrile seizures. Expert Rev Vaccines. 2013 Aug;12(8):885-92. doi: 10.1586/14760584.2013.814781. PMID: 23984960, https://pubmed.ncbi.nlm.nih.gov/23984960/.
[62] Dreier JW, Pedersen CB, Cotsapas C, Christensen J. Childhood seizures and risk of psychiatric disorders in adolescence and early adulthood: a Danish nationwide cohort study. Lancet Child Adolesc Health. 2019 Feb;3(2):99-108. doi: 10.1016/S2352-4642(18)30351-1. Epub 2018 Dec 7. PMID: 30528754; PMCID: PMC6903917. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6903917/
[63] Seneff S, Lauritzen A, Davidson RM, Lentz-Marino L. Is Encephalopathy a Mechanism to Renew Sulfate in Autism? Entropy. 2013; 15(1):372-406. https://doi.org/10.3390/e15010372
[64] Khandaker G, Jung J, Britton PN, King C, Yin JK, Jones CA. Long-term outcomes of infective encephalitis in children: a systematic review and meta-analysis. Dev Med Child Neurol. 2016 Nov;58(11):1108-1115. doi: 10.1111/dmcn.13197. Epub 2016 Jul 16. Erratum in: Dev Med Child Neurol. 2017 Jan;59(1):107. PMID: 27422743. https://pubmed.ncbi.nlm.nih.gov/27422743/.
[65] Wang IJ, Lee PI, Huang LM, Chen CJ, Chen CL, Lee WT. The correlation between neurological evaluations and neurological outcome in acute encephalitis: a hospital-based study. Eur J Paediatr Neurol. 2007 Mar;11(2):63-9. doi: 10.1016/j.ejpn.2006.09.010. Epub 2007 Jan 19. PMID: 17240177. https://pubmed.ncbi.nlm.nih.gov/17240177/ .
[66] Kvam KA, Stahl JP, Chow FC, Soldatos A, Tattevin P, Sejvar J, Mailles A. Outcome and Sequelae of Autoimmune Encephalitis. J Clin Neurol. 2024 Jan;20(1):3-22. doi: 10.3988/jcn.2023.0242. PMID: 38179628; PMCID: PMC10782092. https://pubmed.ncbi.nlm.nih.gov/38179628/.
[67] Kern JK, Geier DA, Sykes LK, Geier MR. Relevance of Neuroinflammation and Encephalitis in Autism. Front Cell Neurosci. 2016 Jan 19;9:519. doi: 10.3389/fncel.2015.00519. PMID: 26834565; PMCID: PMC4717322. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4717322/.
[68] Whiteley P, Marlow B, Kapoor RR, Blagojevic-Stokic N, Sala R. Autoimmune Encephalitis and Autism Spectrum Disorder. Front Psychiatry. 2021 Dec 17;12:775017. doi: 10.3389/fpsyt.2021.775017. PMID: 34975576; PMCID: PMC8718789. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8718789/
[69] Herbert, Martin. Emotional Problems of Development in Children. Internet Archive, Academic Press Inc., 1945, https://archive.org/details/in.ernet.dli.2015.139092/page/n225/mode/2up.
[70] Michaeli O, Kassis I, Shachor-Meyouhas Y, Shahar E, Ravid S. Long-term motor and cognitive outcome of acute encephalitis. Pediatrics. 2014 Mar;133(3):e546-52. doi: 10.1542/peds.2013-3010. Epub 2014 Feb 17. PMID: 24534397. : https://pubmed.ncbi.nlm.nih.gov/24534397/ , https://moscow.sci-hub.se/2755/4ab20e3f3eeed051580baddb4662ba6d/michaeli2014.pdf?download=true
[71] Fowler A, Stödberg T, Eriksson M, Wickström R. Long-term outcomes of acute encephalitis in childhood. Pediatrics. 2010 Oct;126(4):e828-35. doi: 10.1542/peds.2009-3188. Epub 2010 Sep 27. PMID: 20876179. https://pubmed.ncbi.nlm.nih.gov/20876179/.
[72] Mailles A, De Broucker T, Costanzo P, Martinez-Almoyna L, Vaillant V, Stahl JP; Steering Committee and Investigators Group. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis. 2012 May;54(10):1455-64. doi: 10.1093/cid/cis226. Epub 2012 Mar 28. PMID: 22460967. pubmed.ncbi.nlm.nih.gov/22460967/
[73] Pöyhönen HM, Nyman MJ, Peltola VT, Löyttyniemi ES, Lähdesmäki TT. Neuroimaging and neurological outcome of children with acute encephalitis. Dev Med Child Neurol. 2022 Oct;64(10):1262-1269. doi: 10.1111/dmcn.15261. Epub 2022 May 8. PMID: 35527347; PMCID: PMC9545686. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9545686/
[74] Lee WT, Yu TW, Chang WC, Shau WY. Risk factors for postencephalitic epilepsy in children: a hospital-based study in Taiwan. Eur J Paediatr Neurol. 2007 Sep;11(5):302-9. doi: 10.1016/j.ejpn.2007.02.011. Epub 2007 Jun 18. PMID: 17574460. https://pubmed.ncbi.nlm.nih.gov/17574460/.
[75] Rao S, Elkon B, Flett KB, Moss AF, Bernard TJ, Stroud B, Wilson KM. Long-Term Outcomes and Risk Factors Associated With Acute Encephalitis in Children. J Pediatric Infect Dis Soc. 2017 Mar 1;6(1):20-27. doi: 10.1093/jpids/piv075. PMID: 26553786. https://pubmed.ncbi.nlm.nih.gov/26553786/
[76] Hoch, Paul H., and Internet Archive. Psychopathology of Childhood. Internet Archive, New York : Grune & Stratton, 1955. https://archive.org/details/psychopathologyo0000hoch/page/72/mode/2up.
[77] Badawi, Nadia, et al. “Autism Following a History of Newborn Encephalopathy: More than a Coincidence?” Developmental Medicine and Child Neurology, vol. 48, no. 2, 1 Feb. 2006, pp. 85–89, pubmed.ncbi.nlm.nih.gov/16417661/, https://doi.org/10.1017/S001216220600020X.
[78] Srivastava, Vratesh. “Are Unvaccinated Children Healthier?” Vratesh’s Newsletter, 2 Feb. 2023, vratesh.substack.com/p/are-unvaccinated-children-healthier.
[79] United States Court of Federal Claims. “Opinions & Orders | US Court of Federal Claims.” Uscfc.uscourts.gov, uscfc.uscourts.gov/opinions-orders.
[80] PATH. “Case Study: India’s Leadership in the Fight against Japanese Encephalitis.” Www.path.org, www.path.org/who-we-are/programs/center-for-vaccine-innovation-and-access/case-study-indias-leadership-in-the-fight-against-japanese-encephalitis/.
[81] Mudur G. Japanese encephalitis outbreak kills 1300 children in India. BMJ. 2005 Dec 3;331(7528):1288. doi: 10.1136/bmj.331.7528.1288-a. PMID: 16322000; PMCID: PMC1298879. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1298879/
[82] Parida M, Dash PK, Tripathi NK, Ambuj, Sannarangaiah S, Saxena P, Agarwal S, Sahni AK, Singh SP, Rathi AK, Bhargava R, Abhyankar A, Verma SK, Rao PV, Sekhar K. Japanese Encephalitis Outbreak, India, 2005. Emerg Infect Dis. 2006 Sep;12(9):1427-30. doi: 10.3201/eid1209.060200. PMID: 17073095; PMCID: PMC3294746. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3294746/
[83] Puliyel, Jacob. “A Study Tries to Prove Efficacy of a Rotavirus Vaccine That Might Cause More Diarrhoea.” Scroll.in, 20 July 2017, scroll.in/pulse/844323/a-study-tries-to-prove-efficacy-of-a-rotavirus-vaccine-that-might-cause-more-diarrhoea.
[84] ---. “Deaths Reported after Pentavalent Vaccine Compared with Death Reported after Diphtheria-Tetanus-Pertussis Vaccine: An Exploratory Analysis.” Medical Journal of Dr. D.Y. Patil University, vol. 11, no. 2, 1 Mar. 2018, p. 99, pdfs.journals.lww.com/mjdy/2018/11020/Deaths_Reported_after_Pentavalent_Vaccine_Compared.4.pdf?token=method, https://doi.org/10.4103/MJDRDYPU.MJDRDYPU_188_17.
[85] Beet, E. A. “Encephalitis after Yellow Fever Vaccination.” The British Medical Journal, vol. 1, no. 4907, 1955, pp. 226–227, www.jstor.org/stable/20362304.
[86] Roodyn, Leonard. “Encephalitis after Yellow Fever Vaccination.” The British Medical Journal, vol. 2, no. 4898, 1954, pp. 1226–1226, www.jstor.org/stable/20361573?read-now=1#page_scan_tab_contents.
[87] Haas, L. “Encephalitis after Yellow-Fever Vaccination.” The British Medical Journal, vol. 2, no. 4894, 1954, pp. 992–993, www.jstor.org/stable/20330648.
[88] Swift, Sheldon. “Encephalitis after Yellow Fever Vaccination.” The British Medical Journal, vol. 2, no. 4940, 1955, pp. 677–677, www.jstor.org/stable/20332836.
[89] Hargreaves, E. R. “Risks of Immunization.” The British Medical Journal, vol. 2, no. 5148, 1959, pp. 367–367, www.jstor.org/stable/25388425.
[90] Saraswathy, T. S., Zahrin, H. N., Apandi, M. Y., Kurup, D., Rohani, J., Zainah, S., & Khairullah, N. S. (2008). Acute flaccid paralysis surveillance: looking beyond the global poliomyelitis eradication initiative. The Southeast Asian journal of tropical medicine and public health, 39(6), 1033–1039. citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=00b30cc5f15a9a6395c7086b82c634ce8d3475cb.
[91] Michael, B. D., & Solomon, T. (2012). Seizures and encephalitis: clinical features, management, and potential pathophysiologic mechanisms. Epilepsia, 53 Suppl 4, 63–71. https://doi.org/10.1111/j.1528-1167.2012.03615.x, https://onlinelibrary.wiley.com/doi/10.1111/j.1528-1167.2012.03615.x.